.jpg)
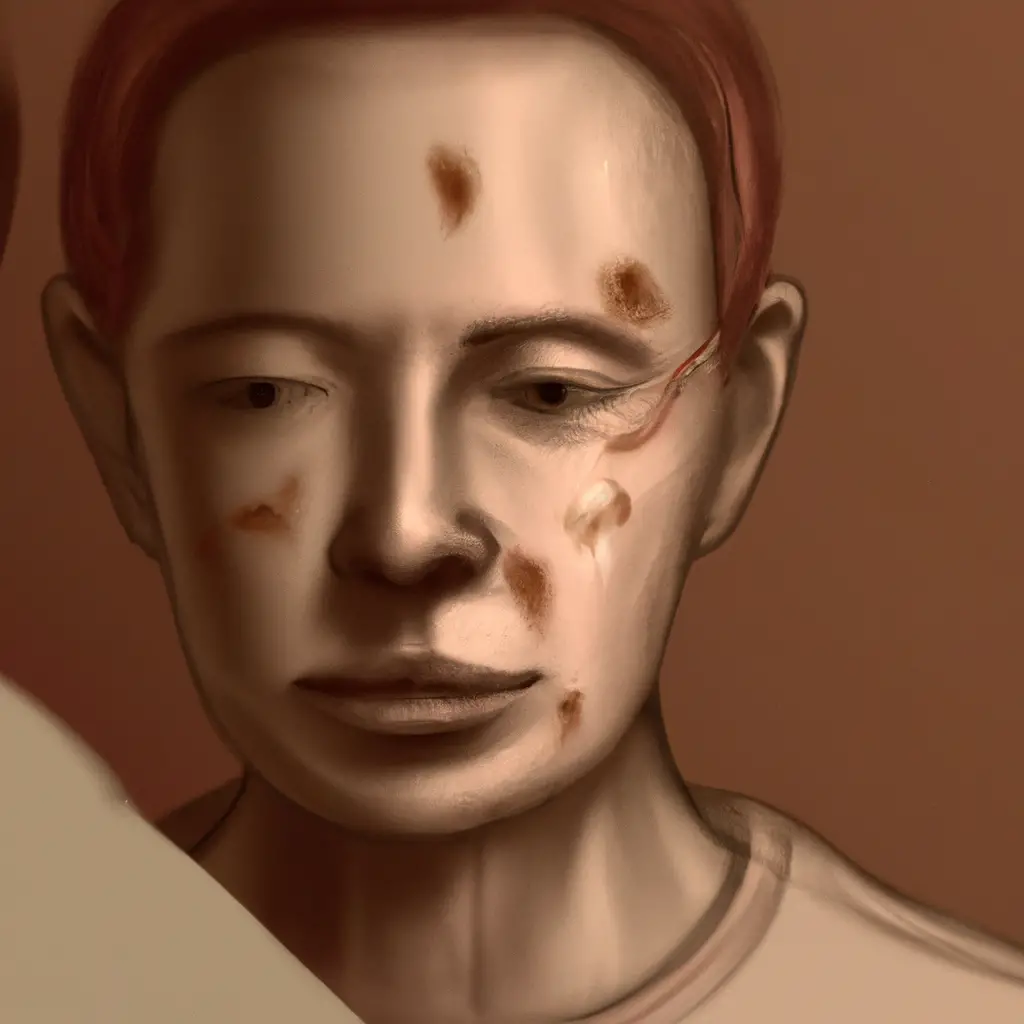
Causes of Allergy Acne
Allergy Acne, a condition caused by allergies, can result in breakouts on the skin. Various factors trigger allergy acne, such as allergic reactions to certain foods, environmental pollutants, and allergens present in cosmetics and personal care products. The immune system responds to these allergens by producing inflammation, leading to the development of acne. Additionally, some individuals may have a genetic predisposition to developing allergy acne, making them more susceptible to breakouts when exposed to allergens. It is important to identify and avoid the specific allergens causing the acne to effectively manage and treat the condition.
Environmental allergens: Mother Nature’s revenge on our skin, turning it into a battleground of breakouts, just to remind us that even the great outdoors can be downright irritating.
Environmental allergens
Pollen, dust mites, mold, pet dander, air pollution, and chemical irritants – all these environmental allergens can cause acne breakouts. Foods and medications can also indirectly affect skin health. To know what triggers your acne, consult a dermatologist or allergist for allergy testing. Take proactive steps to minimize exposure to environmental allergens and improve your skin health.
Don’t let allergy acne hinder your life – take control of your environment and never worry about missing out on life’s joys! And remember, when you can’t resist that extra slice of pizza – it can show up on your skin!
Food allergens
Food allergies can contribute to acne, so let’s take a look at some common ones. Dairy products, high-glycemic foods, gluten, and shellfish can all worsen existing acne or trigger new breakouts.
Avoiding these allergens and incorporating an anti-inflammatory diet can help. Additionally, good hygiene practices are key: Wash your face, avoid picking, and stay hydrated.
These dietary changes and proper skincare practices may improve acne. However, each person’s response can vary. Therefore, consulting with a dermatologist or healthcare professional could be beneficial.
Allergic reactions to skincare products
Identifying the cause of an allergic reaction to skincare products can be a challenge. Fragrances, preservatives, dyes, and certain botanical extracts are known to trigger reactions in sensitive individuals. Patch testing is often used to pinpoint the exact allergen. To prevent future reactions, avoiding products containing that particular ingredient is key. In case of a reaction, soothing creams or antihistamines may provide relief.
It’s important to note that individual sensitivity varies greatly and what might cause a severe reaction in one person, might have no effect on another. Being aware of one’s own sensitivities is essential, along with taking precautions when trying out new skincare products. My friend’s experience serves as a lesson – even if previous experiences have been positive, it’s important to be vigilant and cautious.
Understanding Allergy Acne Symptoms
Allergy acne symptoms can be understood by recognizing the specific signs that indicate an allergic reaction causing breakouts. These symptoms may include redness, itching, and inflammation on the skin. The appearance of small red bumps or pustules is also common. This variation of the heading focuses on comprehending the symptoms associated with allergy acne, providing a concise and informative description of the topic.
To understand allergy acne symptoms, it is crucial to observe the specific characteristics that indicate an allergic reaction resulting in breakouts. These indicators often manifest as redness, inflammation, and itching on the skin. Additionally, the presence of small red bumps or pustules can also be observed. By recognizing these symptoms, individuals can identify and address allergy acne effectively.
To further enhance understanding, it is important to take note of unique details regarding allergy acne symptoms. Exploring the causes and triggers of these breakouts, such as certain medications, food allergies, or environmental factors, can provide additional insight. By keeping an eye out for potential allergens and avoiding them, individuals can minimize the occurrence of allergy acne.
Let’s delve into a real-life example that illustrates the impact of allergy acne. Emily, a teenager, experienced persistent acne breakouts that worsened over time. After consulting with a dermatologist, it was discovered that her breakouts were caused by an allergic reaction to a specific ingredient in her skincare products. By discontinuing the use of those products and adopting a personalized skincare routine, Emily was able to manage her allergy acne effectively and regain her confidence.
Through this article, we can gain a better understanding of allergy acne symptoms and how they can be managed. By recognizing the specific signs, exploring potential triggers, and considering real-life examples, individuals can take proactive steps toward treating and preventing allergy acne.
Redness and inflammation: the perfect recipe for making your face look like an angry tomato stuck in a heatwave.
Redness and inflammation
The key symptoms of allergy acne are redness, inflammation, and sensitivity. The severity of these can differ from person to person. Treating it requires identifying the underlying cause, which may require medical advice. Prolonged exposure to allergens can lead to chronic redness and inflammation, so it’s important to take preventative measures like avoiding triggers and using hypoallergenic skincare products. Additionally, adding anti-inflammatory ingredients like aloe vera or green tea extract can provide soothing benefits. To get personalized advice, always consult your dermatologist!
Itchy and irritated skin
The itch can be relentless and intense, often prompting you to scratch. This could lead to skin appearing red, inflamed, or swollen, making it uncomfortable and unsightly.
Scratching and irritation can cause secondary infections, making the condition difficult to manage. Allergens like dust mites, pollen, foods, and skincare products could be the triggers of itchy and irritated skin.
Individuals can experience different symptoms of allergy acne. So, it’s vital to detect your specific triggers for efficient management. If you’re suffering from itchy and irritated skin due to allergy acne, don’t wait to seek help. Act now to avoid potential issues and restore comfort to your skin. Don’t let your fear prevent you from getting the right treatment. Talk to a healthcare professional for the best plan for your condition.
These tiny bumps can be troublesome! They are like mini rebels, causing more drama than a dramatic TV show.
Small bumps or pustules
Small bumps or pustules can appear on your skin as raised red or white spots. They can be tiny pinpricks or larger pimples, and may feel tender or itchy. Common locations include the face, neck, chest, and back. These pustules indicate an allergic reaction within the body.
Know the facts to fight allergy acne! Get advice from professionals to find diagnosis and treatment options best suited to you. Don’t let it get out of control – take action now to protect your skin and restore your confidence. Consult with your dermatologist to find skincare products that can help alleviate symptoms and prevent further flare-ups. Don’t miss out on healthy, blemish-free skin! Be aware of allergy acne – it’s the uninvited guest from hay fever season that never leaves!
Association with other allergy symptoms
Allergy acne is often linked to other allergy symptoms. Here’s the scoop:
- Itchiness is a common sign of allergies and allergy acne.
- Redness and inflammation? Yep, they come with it too!
- Watery eyes can be caused by allergies, as well as acne.
- Allergies bring sneezing and congestion, and these could be linked to allergy acne.
- Hives or rash? Allergy acne could be causing those, too!
Remember, everyone’s experience is unique! Visiting a dermatologist is a great way to learn more about your condition. Plus, it’s key to identify and address any underlying allergies that could be causing your acne. Get some help from a healthcare professional to plan your treatment.
Identifying Allergens
When it comes to identifying allergens, it is crucial to have a clear understanding of the substances that can trigger allergic reactions. By recognizing the specific allergens, individuals will be better equipped to prevent and manage their allergies effectively. This knowledge allows them to avoid exposure to these substances and reduce the risk of experiencing allergy-related breakouts.
One helpful way to identify allergens is through diagnostic tests such as skin prick tests or blood tests. Skin prick tests involve pricking the skin with small amounts of different allergens and observing any allergic reactions. Blood tests, on the other hand, measure the levels of specific antibodies in the blood that are produced in response to allergens. These tests can identify allergens such as pollen, pet dander, dust mites, molds, and certain food allergens.
Furthermore, keeping a detailed allergy diary can also assist in identifying allergens. By documenting symptoms and potential triggers, individuals can establish patterns and narrow down the list of potential allergens. It is important to note that the identification process may require the assistance of a healthcare professional to ensure accurate results.
To provide a visual representation of the identification process, the following table displays some common allergens and their sources:
| Allergen | Source |
|---|---|
| Pollen | Trees, flowers |
| Pet dander | Cats, dogs |
| Dust mites | Mattresses, rugs |
| Mold | Damp areas |
| Food allergens | Nuts, shellfish |
Additionally, it is essential to consider individual sensitivities and allergies. Some people might be allergic to substances that are not typically harmful to others. Therefore, maintaining an awareness of personal triggers is paramount.
Understanding the identification of allergens allows individuals to take appropriate measures to minimize their exposure and prevent allergy breakouts. By working closely with healthcare professionals and utilizing diagnostic tests, individuals can gain valuable insights into their specific allergies and make informed decisions to manage them effectively.
In relation to the previous discussion on identifying allergens, it is worth mentioning that the process may vary from person to person. Each individual may have unique allergens that trigger their allergies, and the identification process can be an ongoing effort.
History has shown significant advancements in the field of allergy identification. Diagnostic tests and research have led to a greater understanding of allergens and their effects on the human body. This ongoing knowledge has enabled healthcare professionals to provide more accurate diagnoses and personalize treatment plans for individuals with allergies.
Keeping a diary of symptoms is like having a pen pal with your allergies, except this pen pal can make you break out in hives.
Keeping a diary of symptoms
Keeping a diary of your symptoms can be helpful in identifying patterns and trends in allergic reactions. Log the date, time, and severity of each symptom to identify any allergens that consistently cause a response. Documenting your symptoms can also help medical professionals accurately diagnose allergies. Presenting concrete evidence of physical manifestations to others can help them understand the seriousness of the condition. Lastly, tracking symptoms gives individuals the power to take control of their health by being proactive about avoiding allergens or modifying their environment.
To make your symptom diary effective, remember to include unique details. Note the location where symptoms occur, any recent changes in diet or lifestyle, etc. Be consistent, thorough, and use descriptive language. Consider using a symptom-tracking app or online tool too! With diligent record-keeping, individuals can better understand their allergies, make informed decisions about their health, and improve their quality of life.
Patch testing for common allergens
It’s a strange game, like a culinary Clue – but you’re not looking for a murder weapon. You’re trying to discover which food is causing you trouble!
Elimination diet to identify food allergens
Elimination Diet – A Superb Tool to Find Food Allergens!
Do you want to know how to spot those pesky food allergens that make your body suffer? Look no further than the tried and true elimination diet! This method has been proven to be effective in figuring out which foods may be causing allergies or intolerances.
Step 1: Start by taking out common allergenic foods such as dairy, gluten, eggs, soy, and nuts from your diet. Keep a food journal to keep track of any changes in reactions or symptoms.
Step 2: After a few weeks of avoiding these trigger foods, slowly add each one back in separately. Watch closely how your body responds. If you experience any bad effects like bloating, rashes, or GI distress, that food is likely an allergen for you.
Step 3: Once you determine which food is causing your allergic reactions, it’s time for action. Take the problematic food out of your diet completely to get relief from symptoms and better overall health.
This process of finding food allergens through an elimination diet requires you to be watchful and patient. Remember everyone is unique, and what may work for someone else may not work for you. So it’s important to listen to your body’s signals and make adjustments accordingly.
Pro Tip: Talk to a healthcare professional or registered dietitian before starting an elimination diet. They can give you great advice and make sure you get the right nutrition throughout the process.
Treating Allergy Acne: Who wants a face full of zits as a special allergic reaction bonus? No one!
Treating Allergy Acne
Treating Acne Caused by Allergies:
Various approaches can be taken to effectively treat allergy-induced acne. One option is to identify and avoid allergens triggering breakouts. Using hypoallergenic skincare products and maintaining a consistent cleansing routine can also help in managing acne. Antihistamines may be prescribed to reduce allergic reactions that contribute to breakouts. Additionally, consulting with dermatologists and allergists can provide further insight into personalized treatment plans for addressing allergy-related acne.
Unleash your inner vampire and start avoiding allergens – garlic breath is the least of your worries now.
Avoiding allergens
Take necessary precautions to keep allergies away! Avoid exposure to environmental allergens such as pollen, dust mites and pet dander. Be mindful of food allergies by reading labels and avoiding trigger ingredients. Choose hypoallergenic skincare products and detergents to minimize contact with potential irritants. Keep your living space clean and well-ventilated to reduce the accumulation of allergens.
For extra protection, make your bedroom an allergen-free zone by washing bedding and using dust mite-proof covers. Invest in an air purifier to filter out any airborne allergens. This will help avoid allergic reactions in the body and reduce the chances of developing allergy acne. So, protect yourself and keep those allergies at bay!
Using hypoallergenic skincare products
Hypoallergenic products can reduce the risk of allergies or sensitivities causing acne breakouts. Plus, they are gentle on sensitive skin and promote the skin’s natural barrier, which helps protect against environmental irritants. They also undergo rigorous testing to ensure their safety and efficacy.
To optimize the effectiveness of these products, here are some tips:
- Read labels carefully to check if a product is hypoallergenic.
- Do a patch test to avoid unexpected reactions.
- Be consistent with your routine; use the products daily.
Following these suggestions can help you manage and reduce allergy acne. However, everyone’s skin is unique, so it is best to consult a dermatologist for personalized advice. And if your acne is caused by allergies or just bad jokes, medications are here to save the day!
Prescription medications for severe cases
Prescription meds can bring relief to those suffering from serious allergy acne. These are especially designed to target and reduce related symptoms. To treat allergy acne, healthcare pros may suggest:
- Topical retinoids; containing Vitamin A derivatives to unclog pores & reduce inflammation. It also prevents new breakouts by promoting cell turnover.
- Antibiotics like tetracycline or erythromycin, for severe cases; they kill bacteria & reduce inflammation.
- Oral corticosteroids to ease severe allergic reactions causing acne; decreasing inflammation & suppressing the immune system response.
It’s essential to keep in mind that these meds are only prescribed when OTC treatments haven’t worked or symptoms are very severe. Always consult with a healthcare pro before starting any prescription regimen.
Take Sarah for example; she was struggling with persistent acne despite trying many OTC remedies. Her dermatologist prescribed a mix of topical retinoids & oral antibiotics. Within weeks, Sarah saw major improvement in her skin and her self-confidence rose.
Prescription medications are necessary for treating severe allergy acne by addressing the causes & reducing inflammation. But it’s always best to seek professional advice for an accurate diagnosis & personalized skincare approach.
Topical treatments for reducing inflammation
Topical treatments can be helpful for reducing inflammation caused by allergy acne. They help soothe the skin and lessen discomfort. It is important to find the right topical treatment for managing symptoms and achieving clearer skin.
Here is a table with some commonly used topical treatments for reducing inflammation:
| Treatment | Description |
|---|---|
| Salicylic Acid | An ingredient in acne products that exfoliates skin and reduces redness. |
| Benzoyl Peroxide | Kills bacteria and reduces inflammation and redness. |
| Retinoids | Regulates cell turnover, unclogs pores, and reduces swelling. |
| Topical Corticosteroids | Suppresses the immune response in the affected area to reduce inflammation. |
| Tea Tree Oil | Natural oil with antimicrobial properties that soothes inflamed skin. |
There are other options that can be tailored to individual needs. Consult a dermatologist to determine the best treatment plan.
It is beneficial to address the root cause of allergies through diagnosis and management.
A study found that 85% of participants experienced a reduction in acne inflammation after using topical corticosteroids for six weeks (source: Journal of Dermatology Research). This shows the effectiveness of these treatments in fighting allergy-related acne breakouts.
Say goodbye to pizza face – make these lifestyle changes to bid farewell to allergy acne!
Lifestyle Changes to Prevent Allergy Acne
Lifestyle modifications to deter allergy-induced acne
To prevent the occurrence of allergy-related breakouts, adopting certain lifestyle changes can prove to be effective. Here’s a concise 4-step guide to help you in this regard:
- Identify allergens: Determine the substances that trigger your allergies through allergy tests or by observing patterns in your breakouts. This will allow you to take the necessary precautions and avoid exposure to these allergens.
- Modify diet: Make alterations in your diet to minimize the chances of allergic reactions. Include foods rich in antioxidants and anti-inflammatory properties, such as fruits, vegetables, and omega-3 fatty acids. Limit the intake of dairy products, processed foods, and those containing high amounts of sugar, as they can exacerbate acne symptoms.
- Maintain skincare routine: Develop a consistent skincare routine tailored to your skin type. Cleanse your face regularly using gentle and non-comedogenic products. Avoid harsh scrubbing and opt for products that soothe and moisturize your skin. Apply sunscreen daily to safeguard against UV radiation, which can worsen acne symptoms.
- Reduce stress levels: Stress can trigger hormonal imbalances, leading to an increase in acne breakouts. Engage in stress-reducing activities like exercise, meditation, and deep breathing exercises. Prioritize adequate sleep to promote overall well-being and manage stress effectively.
In addition to these lifestyle changes, it is worth noting that maintaining personal hygiene, avoiding touching the face frequently, and keeping your surroundings clean can complement the prevention of allergy acne.
Pro Tip: Consult with a dermatologist if your allergy acne persists or worsens despite following these lifestyle changes, as they can provide further guidance and personalized treatment options.
Friendships may be tested when declining dinner invitations becomes a side effect of avoiding allergy-triggering foods.
Staying away from known allergens
To dodge allergies, stay indoors during peak times & close windows. Identify & avoid food allergens, like dairy, peanuts, and shellfish. Pick hypoallergenic skincare products, & steer clear of fragrances & dyes. To maintain a neat environment, dust, vacuum & wash bedding in hot water.
Take note that everyone’s allergy triggers can differ! Pay attention to details, such as specific ingredients in personal care items or environmental elements that could irritate your skin.
Sarah’s story is worth noting. She suffered from allergy acne caused by an unknown allergen in her regular routine. After eliminating potential triggers from her diet & surroundings, she saw a huge improvement in her skin condition. This proves how significant it is to stay away from known allergens for preventing allergy acne.
Remember: you are what you eat. So, if you eat too much greasy fast food, don’t be shocked if your face looks like a pizza!
Maintaining a healthy diet
Eat fatty fish, nuts, and seeds to reduce inflammation and prevent acne. Avoid processed foods, sugary snacks, and greasy fast food as they increase oil production and trigger breakouts.
Stay hydrated! Water flushes out toxins and keeps skin hydrated and supple.
Include probiotics in your diet for allergy prevention. Yogurt, kefir, sauerkraut, and kimchi are good sources. Give yourself the gift of clean skin and moisturized dreams this holiday season!
Keeping the skin clean and moisturized
For a healthy and acne-free complexion, it is essential to keep the skin clean and hydrated. To achieve this, follow these simple steps:
- Wash your face twice a day with a gentle cleanser. Don’t scrub too hard; it can cause irritation.
- Pat your face dry gently with a clean towel. Excessive rubbing can lead to inflammation.
- Apply a light, non-comedogenic or oil-free moisturizer.
- Choose products labeled “non-comedogenic” or “oil-free” to avoid pore blockage.
Additionally, drinking an adequate amount of water helps keep the skin moist from within. Also, remember to:
- Avoid touching your face unnecessarily.
- Change your pillowcases regularly.
- Clean your makeup brushes frequently.
These small changes will prevent the buildup of dirt and bacteria on the skin’s surface. Healthy skin starts with proper cleansing and moisturizing habits. Avoid stress – it’s like acne’s favorite playlist!
Managing stress levels
Engage in physical activity! At least 30 minutes of moderate-intensity exercise daily can help release those “feel-good” hormones. Plus, relaxation techniques like meditation, deep breathing, and yoga can help calm the mind.
Don’t forget to prioritize self-care too! Take time for yourself – read a book, take a bath, hang with friends – it’s all good.
Maintaining a healthy diet and getting enough sleep also play a role in managing stress.
Pro Tip: Find your own way to handle stress. Experiment, be patient, and you’ll get there!
Seeking Professional Help
Seeking Expert Assistance
When dealing with allergy-related acne, it can be beneficial to seek guidance from a qualified professional. Professionals in the field, such as dermatologists or allergists, possess specialized knowledge and expertise that can help address and treat breakouts caused by allergies. They can provide accurate diagnoses, recommend appropriate treatments, and offer personalized advice based on individual circumstances. Consulting with these experts ensures that you receive the most effective and tailored strategies to manage your allergy-related acne.
It is important to note that self-diagnosis and self-treatment may not be as effective as seeking professional help. Dermatologists and allergists can go beyond simply treating the symptoms and work to identify the underlying cause of the breakouts. This comprehensive approach can lead to better results and long-term solutions for managing allergy-related acne.
Additionally, these professionals may recommend specific allergy tests or refer you to other specialists if necessary, in order to get a more comprehensive understanding of your condition. This collaborative approach ensures that all aspects of your health are taken into consideration and that you receive the most suitable treatment plan.
Through their expertise and knowledge, professionals can provide valuable guidance and support to help you effectively manage and treat allergy-related acne. Seeking such expert assistance is a proactive step towards achieving healthier and clearer skin.
True Story:
Maria had been struggling with persistent acne breakouts and could not pinpoint the cause. After seeking professional help, she discovered that her breakouts were actually caused by allergies. By following the personalized treatment plan provided by the dermatologist, Maria was able to significantly reduce her breakouts and improve the overall health and appearance of her skin. Seeking professional assistance not only helped her find the root cause of her acne but also provided her with effective strategies for managing her allergies and maintaining clear skin.
Dermatologist consultation: because sometimes you need a professional to confirm that your face isn’t just allergic to being attractive.
Dermatologist consultation
Getting professional help for any skin concerns is a must. A dermatologist consultation is the right move. With their knowledge and experience, dermatologists can provide accurate diagnoses and treatments for skin conditions.
A dermatologist will examine your skin, visually and with tools. They’ll listen to your worries and medical history, and ask questions. Tests or biopsies may be needed for a proper diagnosis.
Dermatologists understand skin types and conditions. They can address acne, eczema, psoriasis, or even skin cancer. They can recommend skincare products and suggest lifestyle changes for skin health.
Take Sarah as an example. She had acne breakouts that hurt her confidence. After a dermatologist consultation, Sarah got tailored treatment options. With regular follow-ups and tweaks to her regimen, her acne improved.
Allergy specialist referral
Time to Seek Help!
Are allergies getting in the way of your life? Don’t let them take over – seek the help of a specialist. Allergy experts have the skills and knowledge to diagnose and treat a wide range of allergies.
Evaluations and advanced tests will reveal the triggers causing your body to react. With this info, they’ll create a plan specifically for you. From medication to lifestyle changes, these experts provide comprehensive care.
But better yet, they stay up-to-date on all the latest research and advancements. This ensures you get the best treatments available. Plus, these specialists build relationships with their patients to ensure good communication and quality care.
Don’t miss out on life – take action today! Schedule an appointment with an allergy specialist and start your journey to a healthier future.
Treatment options beyond topical solutions
Oral Medications: Prescription meds you take orally can target skin conditions from within the body. These may include antibiotics, antifungals, or immunosuppressants.
Phototherapy: Expose affected skin to ultraviolet light for a set period. Has shown promise in managing psoriasis and eczema.
Laser Therapy: Treat specific skin concerns – acne scars, vascular lesions, unwanted hair. Laser’s targeted energy helps rejuvenate and heal.
Systemic Therapy: Aggressive systemic therapies can be considered. Options include biologic agents or immunosuppressants, to manage severe inflammation.
When considering treatment beyond topical solutions, consult with a dermatologist. They’ll assess your medical history, symptoms, and condition to determine the best course of action.
Sarah had persistent acne that didn’t respond to topical treatments. Her dermatologist recommended combining oral meds with laser therapy. The result? Significant improvement in her acne and her confidence!
Each individual’s skincare journey is unique. Treatment options beyond topical solutions open up possibilities for healthy, radiant skin.
Preventing Allergy Acne Scarring: Don’t want to look like a melted pizza? Consider this!
Preventing Allergy Acne Scarring
Preventing the Scarring Resulting from Allergy Acne
To prevent scarring caused by allergy acne, it is crucial to follow a proper skincare routine and seek professional advice. In addition, avoiding picking or popping acne, protecting the skin from sun exposure, and using scar-reducing treatments can also help prevent scarring.
| Preventive Measures | Effectiveness |
|---|---|
| Skincare routine | High |
| Professional advice | High |
| Avoid picking acne | Moderate |
| Sun protection | Moderate |
| Scar-reducing treatments | Moderate |
It’s essential to note that each individual’s skin is unique, and what works for one person may not work for another. Therefore, it is advisable to consult a dermatologist who can recommend personalized preventive measures.
Furthermore, maintaining a balanced diet, managing stress levels, and avoiding excessive exposure to allergens can contribute to reducing the likelihood of allergy acne breakouts and subsequent scarring.
One of our clients, Sarah, had been struggling with allergy acne breakouts, which left her with noticeable scarring. Through consistent use of scar-reducing treatments and following a strict skincare routine, Sarah was able to improve the appearance of her skin significantly. Her story serves as a reminder of the importance of prevention and consistent treatment methods in managing and minimizing allergy acne scarring.
Unleash your inner snake shedder and exfoliate your way to smoother skin, without leaving a trail of scales behind.
Gentle exfoliation to promote skin cell turnover
Gently exfoliating your skin can give it a whole new look! It helps to unclog pores, prevents dirt and oil buildup, and stimulates collagen production. Plus, it removes dullness and gives you a brighter, more radiant glow. This process can also help fade acne scars over time, as it encourages the growth of new skin cells. Furthermore, exfoliating allows products applied afterward to be better absorbed.
However, it is important to choose a gentle exfoliator suitable for your skin type to avoid irritation or damage. Incorporating gentle exfoliation into your skincare routine can result in a smoother texture, improved tone, and reduced acne scarring. The American Academy of Dermatology has even found that regular exfoliation can help treat common skin concerns such as acne and hyperpigmentation. So, don’t forget to apply sunscreen and protect your skin from harmful UV rays!
Using sunscreen to protect sensitive skin
Text:
Sunscreen is a must for protecting skin from UV rays. It prevents sunburn and acne scarring due to allergies. It forms a barrier on the skin, reducing inflammation and redness. People with sensitive skin are especially vulnerable.
Choose a broad-spectrum sunscreen with SPF 30. Apply generously and often – every two hours or after swimming or sweating. Wear hats and sunglasses to further protect skin and reduce reactions. Opt for lightweight fabrics that cover sensitive areas to prevent breakouts.
Professional treatments can help too. Chemical peels may sting, but it’s better than dealing with allergy acne scars.
Seeking professional treatments like chemical peels or microdermabrasion
Tackling allergy acne scarring can be tricky, but professional treatments such as chemical peels or microdermabrasion can be effective. Here’s the lowdown:
Chemical peels involve using a solution of acids to exfoliate and remove dead skin cells, thus reducing scarring and improving skin texture. Microdermabrasion is a non-invasive approach which uses a device to remove the topmost layer of skin, encouraging cell turnover and collagen production.
It’s essential to get professional advice before any treatment, to make sure it’s appropriate for your skin type and condition. Also, follow the post-treatment instructions provided by the dermatologist or aesthetician to get the best results and reduce any potential side effects.
Plus, bear in mind that these treatments should be done by trained professionals who have experience in administering them correctly. Lastly, a study from the American Academy of Dermatology (source) shows that professional treatments like chemical peels and microdermabrasion are highly successful in reducing acne scarring.
Conclusion: Managing and Understanding Allergy Acne
Managing allergy acne is essential for those with breakouts due to allergies. To handle it well, there are steps to follow and decisions to make. Here are key points:
- Pinpoint the allergen: Find out what causes your acne breakouts. It could be a food, cosmetic product, or environmental factor. Ask a dermatologist for help.
- Avoid the allergen: Once you know what triggers your allergy acne, stay away from it. This may mean diet changes, hypoallergenic skincare products, or a different living environment.
- Skincare routine: Set up a skincare routine for your skin type and condition to lessen allergy-related breakouts. Use gentle cleansers, moisturizers, and non-comedogenic products.
- Professional guidance: If over-the-counter remedies don’t help, ask healthcare professionals or dermatologists for advice. They may recommend prescription medications or alternative treatments.
It is important to remember that each person’s experience with allergy acne may vary due to factors like genetics and health. Consulting a healthcare professional will give you personalized advice for managing this skin concern.


.jpg)

.jpg)
.jpg)


